Who Should Consider Liver Transplant? Healthtrip Expert Insights
15 Oct, 2025
 Healthtrip
Healthtrip- Identifying Potential Liver Transplant Candidates
- End-Stage Liver Disease: When is a Transplant Necessary?
- The Liver Transplant Evaluation Process at Hospitals like Memorial Sisli Hospital and Fortis Memorial Research Institute, Gurgaon < li>Key Eligibility Criteria for Liver Transplantation
- Absolute and Relative Contraindications to Liver Transplantation
- Liver Transplant Success Stories: Inspiring Examples from Hospitals such as Yanhee International Hospital and Mount Elizabeth Hospital
- Conclusion: Determining if Liver Transplantation is the Right Option, Consider Hospitals like Vejthani Hospital and Saudi German Hospital Cairo, Egypt
Understanding Liver Transplantation
Liver transplantation is a surgical procedure to replace a diseased or damaged liver with a healthy liver from another person. The need for a liver transplant arises when the liver is no longer able to perform its essential functions, like filtering toxins from the blood, producing bile for digestion, and storing energy. End-stage liver disease, or liver failure, can result from a variety of factors, including chronic viral infections like hepatitis B and C, alcohol-related liver disease, non-alcoholic fatty liver disease (NAFLD), genetic conditions like hemochromatosis and Wilson's disease, and autoimmune diseases such as primary biliary cirrhosis and autoimmune hepatitis. When these conditions lead to irreversible damage and liver failure, a transplant becomes a life-saving option. Healthtrip can connect you with experts at hospitals like Memorial Sisli Hospital and Saudi German Hospital Cairo, Egypt to help you understand your condition and explore all available treatment options, including transplantation.
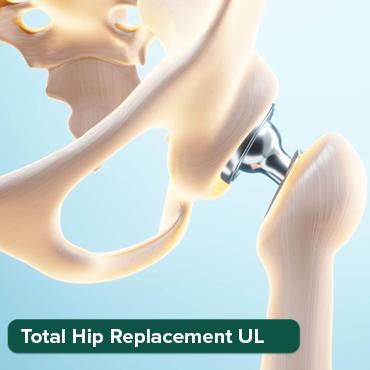
Most popular procedures in India
Who is a Candidate for Liver Transplant?
Determining who is a suitable candidate for a liver transplant involves a comprehensive evaluation process. Generally, individuals with end-stage liver disease who haven't responded to other medical treatments are considered. This includes those with chronic liver diseases like cirrhosis, where the liver is scarred and unable to function correctly. Patients with acute liver failure, a sudden loss of liver function often caused by infections, medications, or toxins, may also be candidates. However, not everyone with liver disease qualifies for a transplant. The evaluation process assesses the severity of the liver disease, the patient's overall health, and their ability to withstand the surgery and post-transplant care. Factors that may disqualify a person include severe heart or lung disease, active infections, uncontrolled psychiatric conditions, or active substance abuse. The assessment is thorough, often involving a multidisciplinary team of specialists at hospitals like Vejthani Hospital and Fortis Hospital, Noida, ensuring the best possible outcomes. Healthtrip can facilitate connections with these top-tier medical centers to streamline the evaluation process.
The Evaluation Process
The evaluation process for a liver transplant is rigorous and thorough, designed to ensure the best possible outcomes for patients. This process typically involves a series of medical, psychological, and social assessments. Doctors will conduct extensive blood tests, imaging studies like CT scans and MRIs, and possibly a liver biopsy to evaluate the extent of liver damage and assess overall health. A cardiologist will evaluate heart function, and a pulmonologist will assess lung health. Psychological and social evaluations are also crucial. Mental health professionals assess the patient's emotional stability and ability to cope with the stress of surgery and post-transplant care, which includes adhering to a strict medication regimen and lifestyle changes. Social workers evaluate the patient's support system and financial resources to ensure they have the necessary support to manage their care after the transplant. Hospitals such as Quironsalud Hospital Murcia and NMC Specialty Hospital, Abu Dhabi have comprehensive transplant programs with experienced teams to guide patients through each step of the evaluation process. Healthtrip assists in connecting patients with these centers, ensuring they receive a comprehensive assessment.
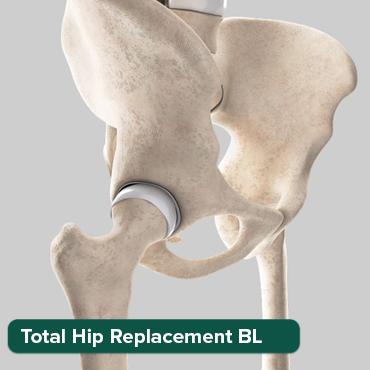
Wellness Treatments
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!
Types of Liver Transplants
There are primarily two main types of liver transplants: deceased donor transplants and living donor transplants. Deceased donor transplants, also known as cadaveric transplants, involve receiving a whole or partial liver from someone who has recently passed away. These organs are carefully matched based on blood type and liver size to ensure compatibility with the recipient. Living donor transplants involve removing a portion of a healthy person's liver and transplanting it into the recipient. This is possible because the liver has the remarkable ability to regenerate, allowing both the donor and recipient livers to grow back to full size. Living donor transplants can reduce waiting times and offer a faster route to transplantation for the recipient. Determining which type of transplant is best suited for a patient depends on several factors, including the severity of their liver disease, their overall health, and the availability of donor organs. Hospitals like Yanhee International Hospital and Fortis Escorts Heart Institute offer both types of liver transplants. Healthtrip can provide information and resources to help patients understand the pros and cons of each option and make an informed decision in consultation with their medical team.
What to Expect After a Liver Transplant
Life after a liver transplant involves a significant commitment to post-operative care and lifestyle adjustments. Immediately following the transplant, patients can expect to spend several days in the intensive care unit (ICU) for close monitoring. As they recover, they'll transition to a regular hospital room for further observation and rehabilitation. One of the most crucial aspects of post-transplant care is managing immunosuppressant medications. These drugs are essential to prevent the body from rejecting the new liver, but they also come with potential side effects, such as increased risk of infection, kidney problems, and high blood pressure. Therefore, regular follow-up appointments with the transplant team are vital to monitor the patient's health and adjust medications as needed. Lifestyle changes are also necessary, including adopting a healthy diet, avoiding alcohol and tobacco, and staying physically active. With proper care and adherence to medical advice, many liver transplant recipients can enjoy a good quality of life for many years. Healthtrip can help connect patients with aftercare and rehabilitation services, ensuring a smooth transition post-transplant with facilities such as Thumbay Hospital and Taoufik Clinic, Tunisia.
Finding the Right Medical Team and Facility
Choosing the right medical team and facility is pivotal to a successful liver transplant journey. Look for transplant centers with a proven track record of successful outcomes, experienced transplant surgeons, and a multidisciplinary team of specialists, including hepatologists, transplant coordinators, nurses, and social workers. It's equally important to consider the hospital's technology, resources, and post-transplant support services. Factors such as the center's waiting times, the availability of living donor transplants, and the range of support programs offered can also influence your decision. Patient testimonials and online reviews can provide valuable insights into the patient experience at different centers. Healthtrip simplifies this process by providing detailed information about leading transplant centers worldwide, like Bangkok Hospital and Memorial Bahçelievler Hospital, including their expertise, facilities, and patient outcomes. We connect you with the best medical teams to ensure you receive personalized care and support throughout your transplant journey, helping you make an informed choice that aligns with your needs and preferences.
Identifying Potential Liver Transplant Candidates
Identifying a potential liver transplant candidate is a multifaceted process, a delicate dance between medical science and human consideration. It's not simply about having a failing liver; it's about determining whether a transplant is the most viable option for improving a patient's quality of life and extending their lifespan. Doctors meticulously evaluate each patient, considering the severity of their liver disease, their overall health, and their commitment to the rigorous post-transplant care regimen. This initial assessment often involves a thorough review of medical history, physical examination, and a battery of diagnostic tests. These tests help to understand the extent of liver damage, assess the function of other vital organs, and rule out any underlying conditions that might compromise the success of the transplant. It's a holistic view, ensuring that the potential benefits of a liver transplant outweigh the risks. Hospitals like Memorial Sisli Hospital, known for their expertise in transplant procedures, have dedicated teams of specialists who work collaboratively to evaluate each candidate, ensuring a fair and comprehensive assessment. They understand that a liver transplant is a life-altering decision, and they approach each case with the utmost care and sensitivity, providing patients with the information and support they need to make informed choices. The journey to transplantation begins with this crucial step of identifying those who stand to benefit most from this incredible medical advancement.
End-Stage Liver Disease: When is a Transplant Necessary?
End-stage liver disease, often a consequence of chronic conditions like cirrhosis, hepatitis, or autoimmune disorders, marks a critical turning point in a patient's health journey. When the liver, our body's tireless workhorse, can no longer perform its vital functions – filtering toxins, producing essential proteins, and aiding in digestion – the consequences can be devastating. Symptoms such as jaundice, ascites (fluid buildup in the abdomen), encephalopathy (confusion and cognitive impairment), and variceal bleeding (bleeding from enlarged veins in the esophagus) become increasingly difficult to manage, significantly impacting the patient's quality of life. At this stage, a liver transplant may be the only hope for survival. The decision to consider a transplant isn't taken lightly. Doctors carefully assess the severity of the liver disease using scoring systems like the Model for End-Stage Liver Disease (MELD) score, which helps to predict survival and prioritize patients on the transplant waiting list. When the MELD score reaches a certain threshold, or when complications of liver disease become unmanageable with conventional medical treatments, a transplant becomes a necessary consideration. It's a moment of reckoning, a recognition that the body's natural defenses have been overwhelmed. Hospitals such as Saudi German Hospital Cairo, Egypt understand the gravity of this situation and offer comprehensive evaluation and treatment options for patients with end-stage liver disease, guiding them through the complex process of deciding whether a liver transplant is the right path forward. The necessity of a transplant is a testament to the severity of the disease, but it also represents a beacon of hope, a chance to reclaim a life stolen by liver failure.
The Liver Transplant Evaluation Process at Hospitals like Memorial Sisli Hospital and Fortis Memorial Research Institute, Gurgaon
Navigating the liver transplant evaluation process can feel like entering a complex maze, but hospitals like Memorial Sisli Hospital and Fortis Memorial Research Institute, Gurgaon, act as experienced guides, providing clarity and support every step of the way. The evaluation isn't just a series of medical tests; it's a comprehensive assessment designed to determine if a transplant is the right course of action for the patient, weighing the potential benefits against the risks. The process typically begins with a detailed review of the patient's medical history, followed by a thorough physical examination and a battery of diagnostic tests. These tests may include blood work to assess liver function, imaging studies like CT scans and MRIs to visualize the liver and surrounding organs, and a liver biopsy to examine the extent of liver damage. Beyond the physical aspects, the evaluation also considers the patient's psychological and social well-being. Transplant teams assess the patient's emotional stability, their ability to adhere to the demanding post-transplant care regimen, and the support system they have in place. Success after a liver transplant requires a strong commitment from the patient and their family, and the evaluation process helps to ensure that they are prepared for the challenges ahead. What sets hospitals like Memorial Sisli Hospital and Fortis Memorial Research Institute, Gurgaon, apart is their multidisciplinary approach. Transplant teams bring together hepatologists, surgeons, psychologists, social workers, and other specialists who collaborate to provide a holistic assessment of each patient. They understand that a liver transplant is a life-changing event, and they approach the evaluation process with compassion and sensitivity, ensuring that patients receive the information and support they need to make informed decisions. It's a journey of discovery, a careful exploration of the patient's health and circumstances, all in the pursuit of the best possible outcome.
Also Read:
Key Eligibility Criteria for Liver Transplantation
Deciding who gets a new liver is a complex balancing act, a blend of medical science and ethical consideration. It's not just about being sick; it's about figuring out who will benefit most from this precious gift. Doctors look at the severity of the liver disease, overall health, and the likelihood of surviving the transplant. They consider factors like age, other medical conditions (heart or lung problems, for instance), and even lifestyle choices. For example, uncontrolled diabetes or severe heart disease might make someone a less suitable candidate because the transplant surgery and the necessary medications can put too much strain on these systems. The goal is to ensure the transplant has the highest chance of success, giving the recipient a longer, healthier life. This often involves a multidisciplinary team of doctors, surgeons, and psychologists who work together to assess each case comprehensively. They also look at factors such as commitment to follow-up care and adherence to medication, crucial for long-term success. Hospitals like Fortis Memorial Research Institute, Gurgaon, meticulously evaluate each patient to determine their eligibility, ensuring a fair and equitable allocation of this life-saving resource. It's a tough process, but one that prioritizes the best possible outcome for everyone involved.
Specific Medical Factors and Considerations
Beyond general health, specific medical criteria play a significant role. The Model for End-Stage Liver Disease (MELD) score is a crucial tool, a numerical representation of the severity of liver disease. It considers bilirubin levels (a measure of liver function), creatinine (kidney function), and INR (a measure of blood clotting ability). A higher MELD score generally indicates a more urgent need for a transplant. But it's not solely about the score. Doctors also consider the specific type of liver disease. Some conditions, like primary sclerosing cholangitis or autoimmune hepatitis, may progress differently and require different considerations. The presence of liver cancer (hepatocellular carcinoma) also presents a unique challenge. While a transplant can be a cure, the cancer must be within specific size and spread criteria to ensure the transplant doesn’t simply allow the cancer to return aggressively. Furthermore, infections, both active and previous, are carefully evaluated. Certain infections can reactivate after a transplant due to the immunosuppressant medications required, potentially leading to serious complications. The transplant team at hospitals like Memorial Sisli Hospital in Istanbul, uses a holistic approach, combining MELD scores with a deep understanding of individual medical histories to make informed decisions.
Also Read:
Absolute and Relative Contraindications to Liver Transplantation
While a liver transplant offers a beacon of hope, it's not the right fit for everyone. There are situations, known as contraindications, where the risks of the surgery and its aftermath outweigh the potential benefits. These fall into two categories: absolute and relative. Absolute contraindications are non-negotiable; if present, a transplant is generally not considered. These can include advanced stages of other serious diseases, such as severe, irreversible heart or lung disease. The rationale is that the stress of the transplant and the subsequent immunosuppression could be fatal. Uncontrolled infections, like active tuberculosis or sepsis, also fall into this category. Transplanting a liver into someone with an active, uncontrolled infection would likely lead to overwhelming complications and death. Similarly, active substance abuse, particularly alcohol or drug dependence, is usually an absolute contraindication. The reason isn't simply moral judgment; it's the high risk of returning to these habits after the transplant, leading to liver damage and transplant failure. Psychiatric conditions that make it impossible for a patient to adhere to the complex post-transplant medication regimen are also considered an absolute contraindication. It's all about ensuring the best possible chance of success, and certain conditions simply make that impossible.
Relative Contraindications: A Matter of Weighing Risks and Benefits
Relative contraindications are less clear-cut. They involve situations where a transplant might still be possible, but only after careful consideration and mitigation of risks. These can include older age. While there's no strict age limit, older individuals may have other health problems that increase the risk of complications. Obesity also presents a challenge. Excess weight can increase surgical risks and make it harder to manage immunosuppression. However, weight loss programs before transplant can sometimes mitigate this risk. Portal vein thrombosis, a blood clot in the main vein that carries blood to the liver, is another relative contraindication. Surgeons may need to perform a more complex operation to bypass the clot and ensure proper blood flow to the new liver. Certain types of liver cancer can also be a relative contraindication depending on size and spread. The decision often involves a careful balancing act, weighing the potential benefits of a transplant against the risks associated with the individual's specific circumstances. Hospitals like Saudi German Hospital Cairo, Egypt, carefully evaluate each patient, considering these relative contraindications in the context of their overall health profile. This allows them to make informed decisions, maximizing the chances of a successful outcome.
Also Read:
Liver Transplant Success Stories: Inspiring Examples from Hospitals such as Yanhee International Hospital and Mount Elizabeth Hospital
Behind the medical jargon and complex procedures, liver transplantation is, at its heart, a story of hope and resilience. It's about individuals facing life-threatening illness who find a second chance through the generosity of organ donation and the skill of medical professionals. These success stories are powerful reminders of the transformative impact of transplantation. Consider the story of a young mother diagnosed with autoimmune hepatitis, her life slowly slipping away as her liver failed. After a transplant at Yanhee International Hospital, she was able to return home to her family, her health restored, and her future bright. Or the tale of a businessman who battled primary biliary cholangitis for years, his energy and vitality diminished. A successful transplant at Mount Elizabeth Hospital allowed him to return to his career and pursue his passions with renewed vigor. These aren't just isolated cases; they represent a growing number of individuals who have been given a new lease on life through liver transplantation.
The Ripple Effect: Impact on Families and Communities
The impact of a successful liver transplant extends far beyond the individual recipient. It ripples outwards, touching families, friends, and communities. When a parent receives a transplant, it means children get to grow up with their love and guidance. When a spouse is restored to health, it strengthens the bonds of marriage and companionship. When a friend overcomes illness, it inspires hope and resilience in others. These stories are often filled with emotion, gratitude, and a profound appreciation for the gift of life. They highlight the importance of organ donation and the dedication of the medical teams who make these miracles possible. Hospitals like Fortis Escorts Heart Institute witness these transformations regularly, seeing patients return to their lives with renewed purpose and a deep sense of gratitude. These success stories serve as a powerful testament to the life-saving potential of liver transplantation and inspire hope for those still waiting for their chance at a healthier future. They underscore the commitment of healthcare professionals to pushing the boundaries of medical science and providing the best possible care to those in need. It also highlights the vital role that patients play in their recovery. Their commitment to follow-up care, adherence to medication, and healthy lifestyle choices are crucial for long-term success.
Also Read:
Conclusion: Determining if Liver Transplantation is the Right Option, Consider Hospitals like Vejthani Hospital and Saudi German Hospital Cairo, Egypt
Deciding whether or not to undergo a liver transplant is one of the most significant decisions a person can make. It's a complex process, involving careful evaluation, weighing risks and benefits, and considering the potential impact on one's life. There's no one-size-fits-all answer; the right choice depends on individual circumstances, medical history, and personal values. However, understanding the eligibility criteria, contraindications, and potential outcomes is crucial for making an informed decision. If you or a loved one is facing end-stage liver disease, exploring the possibility of a transplant is essential. Consult with a qualified medical team, ask questions, and gather as much information as possible. Hospitals like Vejthani Hospital in Thailand and Saudi German Hospital Cairo, Egypt, offer comprehensive transplant programs with experienced professionals who can guide you through the process. Remember, a liver transplant is not a cure-all, but it can be a life-saving option for those who meet the criteria and are committed to the necessary follow-up care. It's a journey that requires courage, resilience, and a strong support system. But for many, it offers a second chance at a healthier, more fulfilling life.
Related Blogs

How Healthtrip Ensures Quality & Safety in Eye Surgery Procedures
Detailed guide on eye surgery, featuring doctors, hospitals, risks, recovery,
End-to-End Logistics for Eye Surgery with Healthtrip's Support
Detailed guide on eye surgery, featuring doctors, hospitals, risks, recovery,
Healthtrip's Care Coordinators: Your Support During Eye Surgery
Detailed guide on eye surgery, featuring doctors, hospitals, risks, recovery,

Top 5 Indian Hospitals for Eye Surgery
Detailed guide on eye surgery, featuring doctors, hospitals, risks, recovery,
Post-Eye Surgery Diet and Lifestyle Tips
Detailed guide on eye surgery, featuring doctors, hospitals, risks, recovery,

Common Risks in Eye Surgery and How Healthtrip Manages Them
Detailed guide on eye surgery, featuring doctors, hospitals, risks, recovery,